Dr. John Stockstill discusses how orthodontics is key to the multidisciplinary, evidence-based approach to diagnosis, and management of sleep-disordered breathing problems
To learn how to treat disease, one must first learn how to diagnose. The diagnosis is the best trump in the scheme of treatment.” — Charcot
It is no wonder that practicing dentists will adopt a method based on the testimonials of a colleague or on unpublished anecdotes and truly believe that they have made an informed decision based on professional judgment. — Dr. Enid Neidle1
Educational aims and objectives
This article aims to explore the multidisciplinary, evidence-based approach to diagnosis,
and management of sleep-disordered breathing problems.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions in the quiz to
earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Identify the role of orthodontics in obstructive sleep apnea (OSA).
- Define the role of orthodontics in the diagnosis of OSA.
- Recognize the role of orthodontics in airway imaging relative to OSA.
- Identifying extraoral and intraoral characteristics of patients with suspected OSA.
- Recognize the role of oral appliances in the treatment of OSA.
Evidence-based (EB) diagnostic and classification strategies for any medically and/or dentally related disorders are intended to weigh the impact of reliability, validity, sensitivity, and specificity derived from the scientific method for techniques and modalities being utilized. The intent of this article is to convey EB diagnostic and classification schemes for obstructive sleep apnea (OSA) in pediatric, pre-adolescent, adolescent, and adult patients seen in the orthodontic office. Additionally, while it is not the intent of this article to comprehensively explore the global neurophysiological nature of sleep disorders, an excellent source of information on this particular subject is available regarding the epidemiology and pathophysiology of sleep disorders, sleep bruxism, and parasomnias often encountered in dental patients.2
What is the role of orthodontics in obstructive sleep apnea (OSA)?
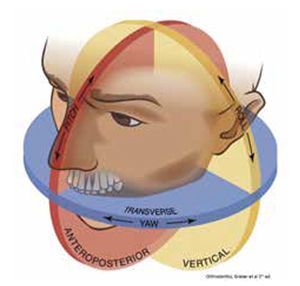
Orthodontics is the art and science of three-dimensional diagnosis and management of 1) dental, 2) skeletal, and/or 3) soft tissue structures of the craniofacial system. Components of diagnosis include documentation of dental, skeletal, and soft tissue relationships relative to one another and to the chief complaint of the patient. Included in this diagnostic work-up is the documentation of posterior airway architecture, including transverse and vertical dimensions of the palatal vault and oropharyngeal areas. This inclusive diagnostic protocol is intended to use orthodontic “gold standards of diagnosis” and to appropriately identify how dentoskeletal and soft tissue findings may correlate with other systemic disorders such as OSA, often overlooked in initial examinations.
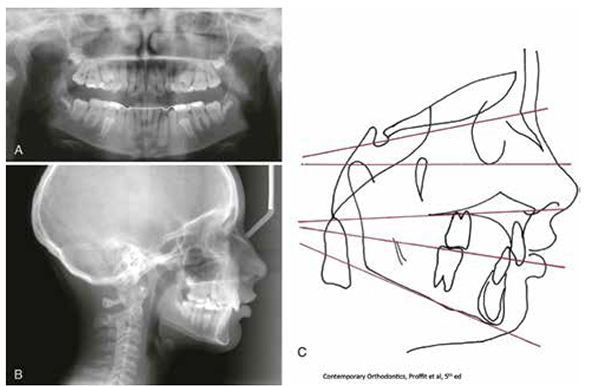
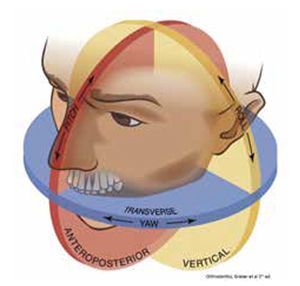
Figure 2: 3 x 3 dimensional planes in orthodontic/OSA diagnosis
OSA is “… a highly prevalent disorder characterized by instability of the upper airway during sleep, which results in markedly reduced (hypopnea) or absent (apnea) airflow at the nose/mouth. Episodes are typically accompanied by oxyhemoglobin desaturation and terminated by brief micro arousals that result in sleep fragmentation and diminished amounts of slow wave and REM sleep.”3 For example, the prevalence of OSA in pediatric patients is the following:
- prevalence of OSA in pediatric population — ~ 2% (NOTE: prevalence in non-syndromic patients)
- parent reported “always snoring” child — 1.5% to 6%
- parent reported apneic events during sleep — 0.2% to 4%
- peak onset between ages 2-8
- “global” sleep-disordered breathing re: parent reported symptoms on questionnaire — 4% to 11%
- prevalence of parent reported snoring by any definition in meta-analysis — 7.45% (95% confidence interval having a range of 5.75-9.8%)4,5
For adults, the prevalence of OSA associated with accompanying daytime sleepiness is approximately 3% to 7% for adult men and 2% to 5% for adult women in the general population.21
OSA or any pulmonary problem is routinely diagnosed and managed by a team of medical personnel including pulmonologists, otorhinolaryngologists, pediatricians, and internists/family physicians. With the evolution of evidence-based OSA diagnostic and management information, it has become commonplace for the medical profession to work closely with their dental colleagues in providing care for these patients. This cooperative or multidisciplinary approach involves not only the appropriate referral of these patients (dentist to physician), but also the proper management of OSA when oral appliances are identified as being potential treatment modalities (physician to dentist). In light of this shared responsibility for our patients, it is imperative that we as clinicians identify key points of clinical protocol for the triage and management of OSA patients. Questions to ask regarding how we as orthodontists should be managing these patients include:
- What is the role of orthodontics in the diagnosis of OSA?
- What is the role of orthodontics in airway imaging relative to OSA?
- What are identifying characteristics of patients with suspected OSA?
- How are treatment decisions made regarding OSA?
- What is the role of oral appliances in the treatment of OSA? Have guidelines been established regarding the use of oral appliances, and is there evidence for their efficacy in general?
What is the role of orthodontics in the diagnosis of OSA?
An appropriate starting point in understanding the characteristics of OSA in our pediatric and adult patients “begins at the beginning.” In craniofacial growth and development, the majority of the cephalocaudal gradient of growth is manifested in the middle-to-lower half of the cranium (nasion/occipitus to menton).6
This significant three-dimensional growth and development of the middle-to-lower half of the cranium chiefly occurs during childhood and puberty, and represents a significant change in facial proportionality during this period.7 In conjunction with the three-dimensional craniofacial development, and in tandem with the development of the mid-face, is the growth and development of the upper airway (most notably, the nasopharyngeal and oropharyngeal components).8
To briefly review, normal development of the airway from embryo to newborn is dependent upon appropriate and timely first and second branchial arch influences along with other factors, including those having to do with genetic penetrance, maternal health and diet, and other external influences. Disturbances in proper growth and development can result in craniofacial syndromes accompanied by airway obstruction or deficiencies in airway architecture. Examples of first and second branchial arch origin syndromes include Down syndrome, Treacher-Collins syndrome, and Pierre Robin Sequence, and, in some instances, cleft lip and palate. All exhibit some degree of airway obstruction as part of their clinical profile. It is within the context of appropriate ortho-dontic diagnosis that this particular component, airway obstruction, be addressed by a multidisciplinary team of dental and medical specialists when these patients are being evaluated.12-13
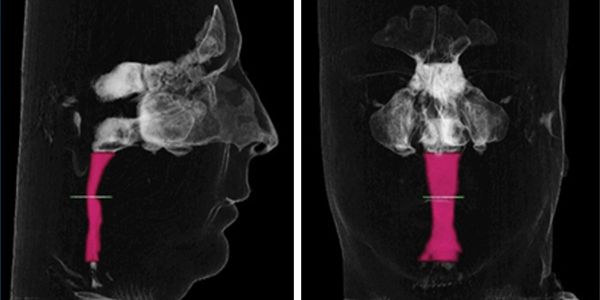
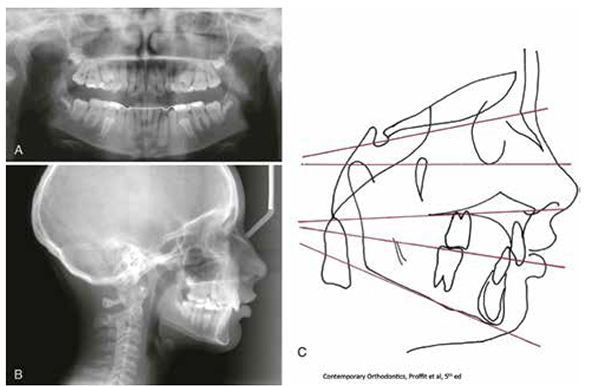
What is the role of orthodontics in airway imaging relative to OSA?
In the past, two-dimensional analysis of the craniofacial region was the “gold standard” for assessing upper airway in orthodontic patients. While somewhat accurate anterior-posterior measurements could be made of the airway using a cephalometric X-ray, no precise analysis could be made since the anatomy of the airway could not be defined in a three-dimensional manner (Figure 1.)
Regarding volumetric analysis of the airway using a two-dimensional image, other limitations exist, including:
- On projecting and converting 3D objects to a reduced two-dimensional image, structures displace vertically and horizontally in proportion to their distance from the film.9,10
- Cephalometric analyses are based on superimposition of the left and right sides at mid-sagittal plane, but precise superimposition is difficult to achieve since facial symmetry is infrequent.
- Manual data collection and processing (manual and digital representation of physical landmarks) in cephalometric analysis have been shown to be less precise than three-dimensional imaging techniques.
- Errors in cephalometric measurements may be associated with uncertainties in locating anatomical landmarks due to the deficiency of well-defined outlines, hard edges, and shadows as well as patient position, and due to operator error, especially in the absence of acceptable intrarater and, when utilized, interrater reliability.11
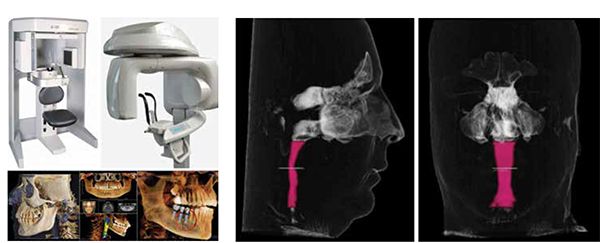
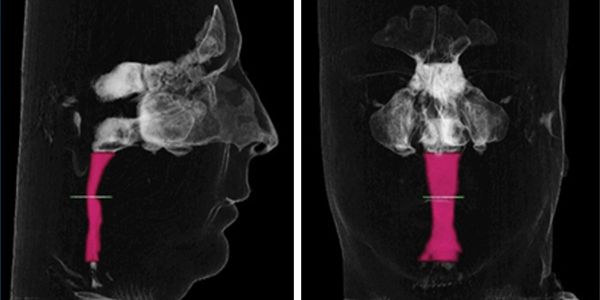
The greatest limitation of a two-dimensional technique is the inability of the cephalometric X-ray to adequately address volumetric analysis of the airway. That is, the transverse dimension of the airway cannot be seen in the field of imaging, and thus, any assessment of the airway volume using two-dimensional imaging would be inadequate and incomplete. With the advent of three-dimensional imaging capability observed in cone beam computerized tomography (CBCT), a true three-dimensional volumetric analysis of the upper airway is possible and is now used as an adjunctive diagnostic modality in the comprehensive orthodontic evaluation of suspected OSA cases.9-11
As a result of this imaging improvement, the orthodontist is now able to evaluate not only dental, skeletal and soft tissue structures in a three-dimensional (x – y – z) dimension, but also capable of evaluating the integrity of these structures relative to their pitch (coronal or anterior-posterior dimension), yaw (transverse or horizontal dimension), and roll (vertical or sagittal dimension) (Figure 2).
Thus a “true 3 x 3 dimensional analysis” allows the orthodontist to more accurately diagnose dental, skeletal, soft tissue, AND upper airway dimensions as needed (Figures 3A-3B).
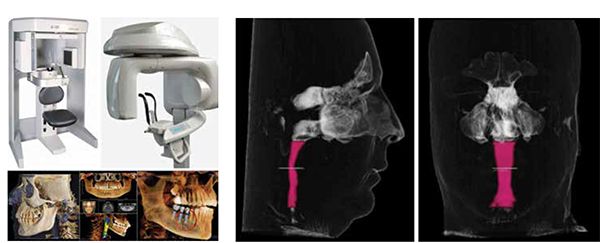
(From left) Figure 3A: CBCT for imaging airway — adjunctive for three-dimensional diagnosis; Figure 3B: Advanced CBCT orthodontic imaging — anterior-posterior and transverse airway imaging. 3D airway evaluation
What are identifying extraoral and intraoral characteristics of patients with suspected OSA?
A comprehensive orthodontic examination includes the observation, measurement, and documentation of dental, skeletal, and soft tissue components of the craniofacial region. With the advent of interest in sleep-disordered breathing and its diagnosis and management, more attention is being given to breathing and respiration integrity when collecting clinically useful data for orthodontic diagnosis. Specifically, documentation of the anatomical architecture and integrity of the oropharyngeal area, including the tonsils and tonsillar crypts, base of tongue, and tongue position should be a part of a comprehensive orthodontic records appointment. Other physical characteristics routinely observed during an appointment and exhibited by suspected OSA patients include:
- Neck girth (circumference) > 17 inches (physical assessment by physician)
- Retropositioned mandible (Class II skeletal profile)
- Retropositioned maxilla
- Vaulted or narrowed palate — transverse palatal constriction
- Enlarged tongue relative to arch forms with scalloping of the lateral surfaces of the tongue suggestive of tongue thrust behavior
- Inferiorly positioned hyoid bone relative to the mandibular border
- Chronic mouth breathing
- Elevated Mallampati score (3-4)
- Subjective report of the following:
- Daytime sleepiness
- Difficulty concentrating upon everyday tasks, including attention deficit hyperactivity (ADHD)
- Waking up “feeling tired”
- History of upper respiratory disorders, including eustachian tube problems (“tubes in ears”), asthma, respiratory allergies
- Diagnosed obesity
- Generalized parasomnias co-morbid with sleep bruxism, including restless leg syndrome, sleep walking, enuresis, and gastroesophageal reflux (GERD)2,14
The most frequent physical findings on examination of suspected OSA or sleep-disordered breathing patients are:
- Narrow maxilla (reduced transverse palatal width)
- Posterior cross bite (bilateral more severe than unilateral re: OSA patients)
- Forward tongue posture during rest and during swallowing (“lick your lips, and let your jaw relax”)
- Juvenile tongue thrust in swallowing (anteriorly projected rather than against palatal rugae)
- Hypertrophied tonsillar crypt areas
- Subjective parental report of “snoring” and “interrupted breathing during sleep” — report of suspected apneic episodes by parent or “bedroom report”
Given the physical signs and subjective symptomatology common to OSA, it is apparent that a very thorough extraoral and intraoral craniofacial examination be conducted as part of the orthodontist’s diagnostic due diligence to their patients.
How are treatment decisions made regarding OSA?
Management of OSA is a multi-disciplinary effort utilizing a number of treatment modalities such as CPAP (continuous positive airway pressure – nasal or oral); behavior modification (dietary modifications, smoking cessation, weight loss, and exercise, for example); MME (maxillomandibular surgical expansion/advancement); and oral appliances. The “gold standard” for reliably and accurately diagnosing OSA is polysomnography (sleep study – PSG) conducted either in medical facilities such as “Sleep Centers” or a home study utilizing a portable polysomnography unit. Data collection includes electroencephalogram (EEG) activity to measure and record brain wave activity, electromyography (EMG) to record muscle movements associated with restless leg movements and sleep bruxing, electrooculogram (EOG) to record eye movements during REM-NonREM transitions during sleep, electrocardiogram (ECG) to record heart rate, nasal air flow sensors, and audio microphones to record frequency and duration of snoring.15 The physician ordering the PSG interprets the data collected, and treatment recommendations are made according to the severity of the problem, most often using the “gold standard” of Apnea-Hypopnea Index (AHI) and blood oxygen saturation. Sometimes, Respiratory Disturbance Index (RDI) is used to classify OSA, but this may be somewhat confusing since it includes data other than AHI, resulting in the RDI being greater than the standard AHI. By definition, apnea is the complete cessation of airflow for at least 10 seconds, and these can be classified as obstructive, central, or mixed based on whether effort to breathe is present during the event. Hypopnea is defined as a reduction in airflow that is followed by an arousal from sleep or a decrease in oxy-hemoglobin saturation21.
Using AHI findings for treatment recommendations, the severity of OSA is classified as:
- None/Minimal: AHI < 5 per hour
- Mild: AHI ≥ 5, but < 15 per hour
- Moderate: AHI ≥ 15, but < 30 per hour
- Severe: AHI ≥ 30 per hour
What is the role of oral appliances in the treatment of OSA? Have guidelines been established regarding the use of oral appliances, and is their evidence for their efficacy in general?
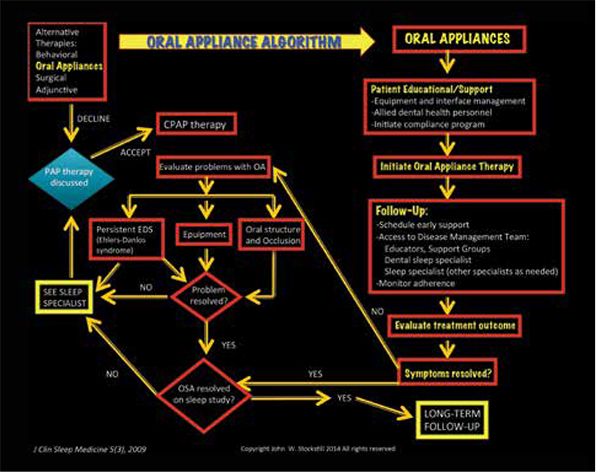
It has been reported that oral appliances are more efficacious in treating patients having AHI scores of < 5 per hour (none/minimal) to AHI scores of > 15 but < 30 per hour.16,17 Oral appliances to be used during sleep are usually designed to have full arch coverage in the maxilla and mandible for mandibular repositioning. With this design, the maxilla acts as an anchor to the protrusive repositioning of the mandible, and the mandible and tongue are held forward (protrusively) to improve posterior airway patency with the patient in a supine sleeping position. Tongue retention appliances are designed for both arches (discussed previously) if tongue retention is desired while protrusively repositioning the mandible.18 In patients exhibiting more severe OSA, the use of the CPAP or MME is recommended. CPAP is considered reversible therapy as are the oral appliances, but patients using the CPAP or oral appliances must be periodically monitored for any changes in dental occlusal relationships and/or temporomandibular joint integrity. MME is an irreversible surgical correction protrusively repositioning both the maxilla and mandible in order to improve nasal and oral airway patency (to be discussed in “Orthodontic diagnosis and management of OSA: part 2 — case presentations”). An algorithm and flow chart for recommended treatments and referrals can be seen in Figure 4.9
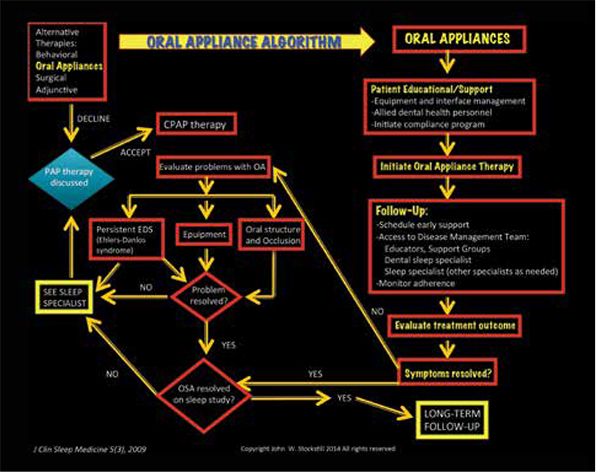
Figure 4:Initiation, management, and follow-up of oral appliances
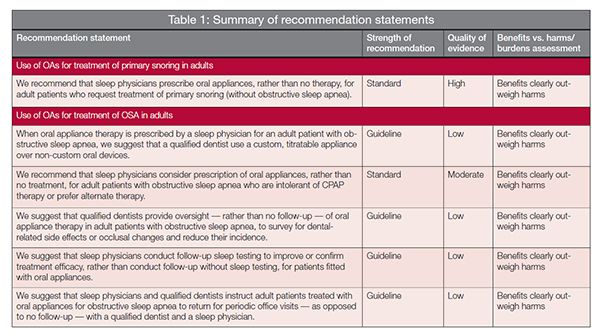
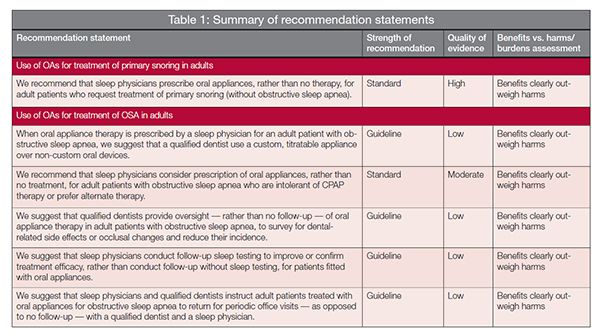
Guidelines for and definition of effective oral appliances for the treatment of obstructive sleep apnea and snoring of the American Academy of Dental Sleep Medicine (AADSM)(2014) are listed in Table 1. This generalized description of the “what, how, and why” of oral appliance therapy was an attempt to lay the groundwork for establishing an evidence-based “gold standard” for appliance use in treating OSA. To summarize this attempt at standardization of treatment, it was agreed that oral appliances:
- treat OSA, primary snoring, and associated symptoms
- decrease the frequency and/or duration of apneas, hypopneas, respiratory effort-related arousals (RERAs), and/or snoring events
- improve nocturnal oxygenation as well as the adverse health and social consequences of OSA and snoring
- are indicated for patients with mild to moderate OSA and primary snoring
- should be used in treatment of patients with severe OSA who do not respond to or are unable or unwilling to tolerate positive airway pressure (PAP) therapies
- are an adjunct to PAP therapy and/or other treatment modalities for the management of OSA
- mandibular advancement devices are the most effective and widely used in clinical practice
Orthodontics is recognized as being a key player in the multidisciplinary, evidence-based approach to diagnosis and management of sleep-disordered breathing problems ….
Recently, a collaboration between the American Academy of Sleep Medicine and the American Academy of Dental Sleep Medicine resulted in the publication of Clinical Practice Guideline for the Treatment of Obstructive Sleep Apnea and Snoring with Oral Appliance Therapy: An Update for 2015 – An American Academy of Sleep Medicine and American Academy of Dental Sleep Medicine Clinical Practice Guideline. These guidelines include recommendations for the use of oral appliance therapy in the treatment of OSA and snoring, and are internally graded as to their strength of recommendation, quality of evidence and benefits versus harms/burdens assessment. These guidelines represent the best effort to date to identify for whom and how these appliances should be implemented for the treatment of OSA and snoring.
As a supplement to the listed guidelines and recommendations, the AADSM published a list of Functional Expectations of Oral Appliances in 2014 with emphasis placed upon the limitations of these appliances and the specifications for their fabrication and use.
- OAs are fabricated to protrude and help stabilize the mandible in order to maintain a patent upper airway during sleep.
- An OA is custom fabricated using digital or physical impressions and models of an individual patient’s oral structures.
- An effective OA is NOT a prefabricated item that is trimmed, bent, relined, or otherwise modified.
- An OA is made of biocompatible materials and engages BOTH the maxillary and mandibular arches.
- OAs allow the mandible to be advanced in increments of < 1 mm with protrusive adjustment range of 5 mm.
- Any reversal of the mandibular advancement must be possible.
- OAs are suitable for placement and removal by the patient or caregiver.
- OAs maintain a stable retentive relationship to the teeth, implants, or edentulous ridge and retain the prescribed setting during use
- OAs maintain their structural integrity over a minimum of 3 years.
These expectations and limitations were developed as a means of establishing some sense of evidence-based uniformity in the fabrication and use of oral appliances with OSA patients for dental generalists and specialists.
Conclusion
Orthodontic diagnosis is a three-dimensional exercise in data collection including advanced CBCT imaging and digitally scanned models that help provide the orthodontist with cutting edge information about their patients. In the past, orthodontic diagnosis consisted of data specific for dental, skeletal, and soft tissue structures and relationships. However, current standards for diagnosis and treatment may now include airway architecture analysis, diagnosis of sleep-disordered breathing and management strategies for OSA diagnosed in pediatric and adult patient populations alike. Orthodontics is recognized as being a key player in the multidisciplinary, evidence-based approach to diagnosis and management of sleep-disordered breathing problems and how these problems relate to the growth, development, health, and well-being of our orthodontic patients.